IUI
- Home
- IUI
IUI
Intrauterine insemination (IUI) is a fertility treatment that involves injecting sperm directly into the uterus to help increase the chances of pregnancy.
Q. What is IUI?
Intrauterine insemination (IUI) is a first-line and low-cost fertility treatment that offers hope to couples or individuals struggling with infertility. The procedure involves placing best sperms (with highest motility after washing) directly into a woman’s uterus around the time of ovulation to increase the chances of fertilization. IUI is considered less invasive and more affordable compared to other assisted reproductive technologies such as in vitro fertilization (IVF) and ICSI.
Q. What are the indications of IUI?
(i) Unexplained infertility
(ii) mild male-factor infertility
(iii) cervical mucus issues
(iv) minimal and mild endometriosis
(v) anovulatory cycles like in PCOS
Q. What are the success rates of IUI in one-cycle?
Success rates vary depending on factors such as age, underlying fertility issues, and the use of fertility medications. On average, the success rate per IUI cycle ranges between 10% to 20%.
Q.Are there any side – effects related to IUI procedure?
While IUI is generally safe, some risks include multiple pregnancies and OHSS (when fertility drugs are used for egg formation) and minor discomfort during the procedure.
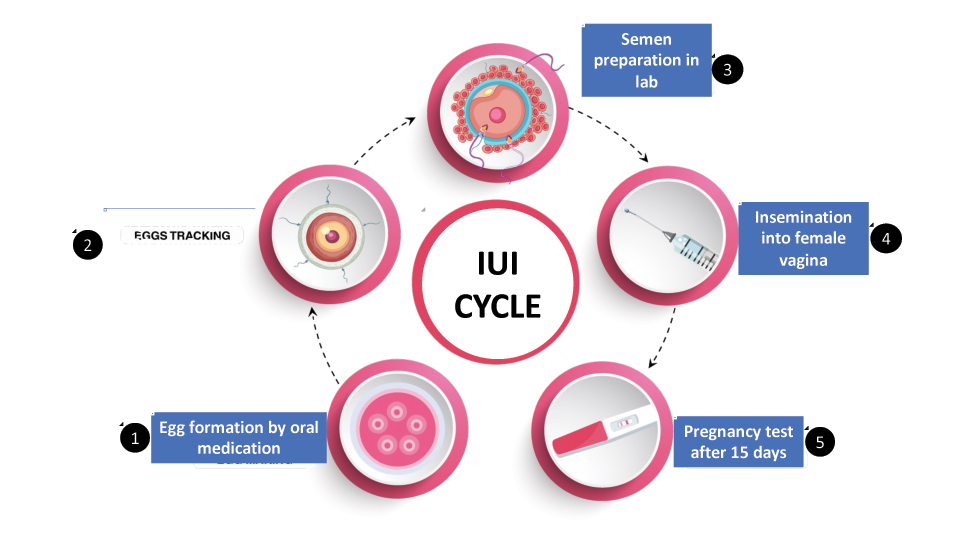
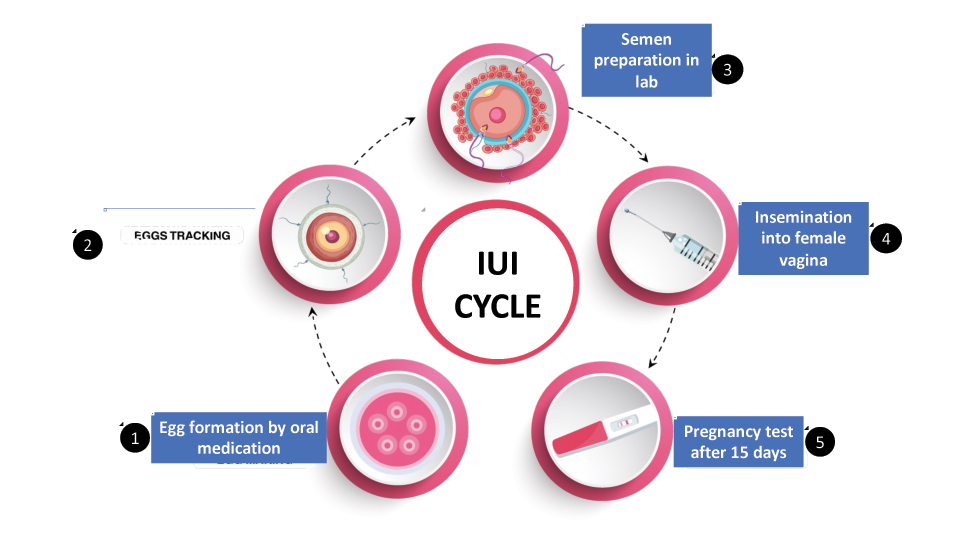
Q. What are the steps involved in IUI?
(i) Initial Consultation and Evaluation
(1 a) Before the IUI procedure, both partners undergo a simultaneous fertility evaluation. This may include blood tests for hormones, female pelvic ultrasound, and semen analysis.
(1 b) The woman’s menstrual cycle is monitored to determine when she ovulates. This can involve tracking her natural cycle or inducing ovulation with medication.
(ii) Ovulation Induction/ egg-formation
(2 a) Some women may take fertility medications, such as clomiphene citrate/letrozole or injectable hormones, to stimulate the ovaries to produce more than one egg, increasing the chances of conception.
(2 b) Frequent ultrasounds and blood tests monitor the development of follicles (which contain the eggs) in the ovaries to pinpoint the best time for insemination.
(iii) Monitoring Ovulation
(3 a)Once the follicles mature, ovulation is closely tracked. This can be done through ultrasound or with an ovulation predictor kit that measures the luteinizing hormone (LH) surge, which indicates ovulation is imminent.
(3 b) In some cases, an injection of human chorionic gonadotropin (hCG) is administered to trigger ovulation if it does not happen naturally.
(iv) Sperm Collection and Preparation
(4 a) On the day of insemination, the male partner provides a sperm sample (by masturbation), or donor sperm is used.
(4 b)The sperm sample is “washed” in a lab to separate healthy, motile sperm from the seminal fluid and other debris. This concentrates the best sperm for insemination, which improves the chances of success.
(v) Insemination Procedure
(5 a) The prepared sperm sample is placed into a thin, flexible catheter.
(5 b) The woman lies on an examination table, and the catheter is gently inserted through the cervix into the uterus. The sperm is injected directly into the uterus, which helps them reach the fallopian tubes where fertilization may occur.
(vi) Post-Procedure
(6 a) After the insemination, the woman may rest for a short time (10-15 min) before resuming normal activities.
(6 b) Two weeks after the procedure, a pregnancy test is done to determine if the IUI was successful